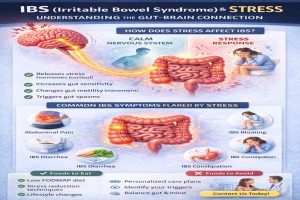
IBS (Irritable Bowel Syndrome) and Stress: Understanding the Gut-Brain Connection
BS (Irritable Bowel Syndrome) is one of the most common digestive disorders, affecting millions of people worldwide. Many patients notice
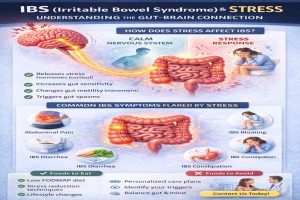
BS (Irritable Bowel Syndrome) is one of the most common digestive disorders, affecting millions of people worldwide. Many patients notice

Causes of post-colonoscopy bleeding can range from minor issues to more serious conditions, and understanding these can help you gauge your situation. After a colonoscopy, it’s vital to recognize what constitutes normal recovery and when you should seek medical attention. If you experience any unexpected bleeding, knowing the potential factors can alleviate your concerns and assist you in making informed decisions about your digestive health. Do not forget if you’re unsure about your symptoms. It’s always best to consult your gastroenterologist, Dr. Karim Shakoor, for personalized advice.
Before you undergo a colonoscopy, it’s imperative to understand what the procedure entails.
With a colonoscopy, your gastroenterologist examines the lining of your colon and rectum using a flexible tube equipped with a camera. This outpatient procedure typically takes 30 to 60 minutes and allows for the detection of abnormalities in your digestive tract.
A colonoscopy is critical in preventive health care and the early detection of bowel diseases. It is primarily used to screen for colorectal cancer, identify polyps, and diagnose conditions such as inflammatory bowel disease (IBD) or diverticulitis.
Colonoscopy is a vital tool for maintaining digestive health. It identifies potential issues before they become serious. Regular screenings can significantly reduce your risk of developing colorectal cancer by allowing for the timely removal of polyps and abnormalities.
Understanding the different colonoscopy types can help you appropriately prepare for your procedure. Here are the main types:
After your procedure, your gastroenterologist will discuss findings and further actions if necessary.
Type of colonoscopy | Description |
Standard Colonoscopy | Invasive examination of the entire colon. |
Virtual colonoscopy | This is a non-invasive imaging technique that uses CT scans. |
Diagnostic Colonoscopy | This is Conducted to investigate symptoms or abnormalities. |
Therapeutic Colonoscopy | This is Used for treatment, such as removing polyps. |
Flexible Sigmoidoscopy | Focuses on the rectum and lower part of the colon. |
Understanding the different types of colonoscopy enables you to have informed discussions with your doctor about which procedure is best for your needs. After the procedure, your gastroenterologist will provide detailed insights into your digestive health.
Colonoscopy plays a crucial role in preventive mechanisms for colorectal health. You can take proactive steps to ensure your long-term health by identifying and addressing issues quickly.
Although the colonoscopy procedure is generally safe, it can have side effects like any medical intervention. Knowing these potential outcomes helps ensure you know what to expect and when to seek further medical advice.
Side effects such as minor bleeding can occur after a colonoscopy, especially if polyps are removed during the procedure. While some blood in your stool may be normal, significant bleeding is not and should be promptly evaluated by your healthcare provider.
One common side effect after a colonoscopy is abdominal discomfort, which may include cramping or bloating. This is usually temporary and should resolve within a few hours as the anesthesia wears off and your body adjusts.
This abdominal discomfort is often due to the air introduced into your colon during the procedure. As your body expels this air, you may feel slight pain or a sensation of fullness. Still, these symptoms typically lessen with time, allowing you to return to normal activities.
Any colonoscopy can cause feelings of gas and bloating, which are common complaints after the procedure. This discomfort is usually due to the air inflation of the colon during the examination.
Understanding that the introduction of air into your digestive system is a necessary part of the colonoscopy can help ease your concerns. This sensation generally subsides as you pass gas, so take your time and allow your body to recover naturally. If you experience prolonged bloating or severe pain, it’s advisable to consult your healthcare provider.
Understanding the potential causes of post-colonoscopy bleeding is crucial for your health. Various factors can contribute to this complication, some linked to the procedures performed during the colonoscopy.
Any time a polyp is removed during a colonoscopy, there is a risk of bleeding. Although this is a common practice to prevent possible future complications, it can lead to temporary bleeding that typically resolves independently.
Post-colonoscopy bleeding can also arise from complications related to biopsies taken during the procedure. These biopsies are crucial for diagnosing various gastrointestinal conditions but can occasionally lead to unanticipated bleeding.
For instance, the act of taking a biopsy involves cutting tissue, which may disrupt blood vessels and result in bleeding. While serious complications are rare, knowing this risk helps you monitor your recovery more effectively.
One significant factor in post-colonoscopy bleeding is your pre-existing medical conditions. Certain health issues, such as clotting disorders or gastrointestinal diseases, can increase your susceptibility to bleeding after the procedure.
Plus, having conditions like liver disease or taking anticoagulants (blood thinners) may exacerbate the bleeding risk, making it crucial to discuss these with your healthcare provider before your colonoscopy.
Biopsy assessments also play a vital role in determining how your medical history influences post-colonoscopy complications. Knowing your medical background helps your doctor make informed decisions during the procedure.
Pre-existing health conditions and medications can significantly impact your recovery, reinforcing the importance of an open dialogue with your gastroenterologist regarding your full medical history before undergoing a colonoscopy.
To ensure your health and safety after a colonoscopy, it’s crucial to recognize the signs of severe symptoms that may indicate complications. Knowing these symptoms can help you determine when to seek immediate medical attention.
Blood in your stool can vary significantly after a colonoscopy. If you notice a small amount of bright red blood, it may not be a cause for concern. However, if you experience large amounts of dark red or maroon blood, this could indicate a more serious issue that requires prompt medical evaluation.
Recognizing additional symptoms that accompany any bleeding is imperative for assessing your situation. Symptoms such as severe abdominal pain, dizziness, or fainting should always be taken seriously. They may indicate that you must contact your doctor or visit the emergency room.
Accompanying symptoms can provide vital clues about the severity of your condition. These signals should not be ignored if you experience sudden changes in your health, like increased pain or unusual fatigue. The presence of chills or fever, alongside gastrointestinal bleeding, can also indicate an infection or other complications.
An important factor to consider is the duration of the bleeding. Minor bleeding that resolves within a day or two is not a cause for concern. However, if the bleeding persists for more than a couple of days, it is crucial to contact your healthcare provider for further assessment.
Severe and ongoing bleeding can signify complications related to the colonoscopy. If you notice that bleeding continues without improvement or worsens over time, you must seek medical assistance. Prompt attention can help prevent further complications and ensure your digestive health remains intact.
Once again, it is important to recognize the signs that indicate you should seek medical attention after a colonoscopy. While minor bleeding or discomfort can be expected, there are specific symptoms that warrant prompt evaluation.
With any post-procedural symptoms such as significant abdominal pain, persistent bleeding, or fainting, you should contact your healthcare provider immediately. These could be indications of a more serious complication following your colonoscopy.
The importance of knowing whom to call in an emergency cannot be overstated. Keep your gastroenterologist’s contact information and the nearest emergency room numbers accessible should urgent care be necessary.
Though rare, complications that can arise from a colonoscopy include perforation, heavy bleeding, or infection. In these cases, you may need to seek help from your gastroenterologist, such as Dr. Karim Shakoor at Colon and Digestive Health in Conyers, GA, or visit a nearby emergency department. This readily available information ensures you can act quickly if you experience any troubling symptoms.
Your post-procedure plan should include contacts for follow-up care. A follow-up appointment with your gastroenterologist is crucial to confirm your recovery and address any lingering concerns.
To ensure a smooth recovery, schedule a follow-up visit within a week or as directed by your doctor. During this appointment, communicate any unusual symptoms you have experienced since your colonoscopy, allowing your healthcare provider to assess your overall digestive health effectively. Note that staying proactive about your health is important, especially after procedures like colonoscopies.
Unlike many medical procedures, the success of a colonoscopy significantly depends on your preparation and care both before and after the examination. Taking the right steps can reduce your risk of complications and enhance your overall digestive health.
Preventive measures begin with proper preparation for your colonoscopy. This typically involves following a specific diet, including a clear liquid regimen a day before the procedure, and using prescribed laxatives to help cleanse your colon. Following your gastroenterologist’s instructions, like those provided by Karim Shakoor, M.D. at Colon and Digestive Health in Conyers, GA, is crucial for a successful procedure.
A crucial part of diligent recovery is following post-procedure care instructively. After your colonoscopy, you may experience mild discomfort. Still, monitoring your body for any unusual symptoms, such as significant pain or bleeding, is vital.
Some bloating and gas post-colonoscopy are normal, but you should monitor your bowel movements. If you notice rectal bleeding that lasts more than a few days or if you experience a fever, contact your gastroenterologist immediately. Proper hydration and gradually reintroducing your diet can also aid in recovery.
Colonoscopy recovery doesn’t just end with the procedure; lifestyle adjustments can greatly enhance your digestive health. Incorporating fiber into your diet, staying hydrated, and maintaining a regular exercise routine can help promote optimal gastrointestinal function.
Adjustments like minimizing red meat and processed foods while increasing fruits, vegetables, and whole grains can significantly improve overall well-being. These changes, combined with regular screenings at reliable clinics like Colon and Digestive Health in Conyers, GA, can contribute to better digestive health and earlier detection of potential issues.
So, if you experience post-colonoscopy bleeding, it’s typically due to the removal of polyps, biopsies, or minor tears in the bowel. While some spotting can be normal, you should be concerned if the bleeding is heavy, continues for more than a few days, or is accompanied by severe pain or fever. Always consult your gastroenterologist for guidance to ensure your recovery is on track. For more information, contact your local colonoscopy clinic and discuss any lingering worries regarding your digestive health.
A: Post-colonoscopy bleeding can occur for several reasons. The most common causes include the removal of polyps or biopsies taken during the procedure, irritation of the bowel lining from the colonoscope, or existing bleeding disorders. Bleeding may also result from perforation of the bowel, though this is rare. Most bleeding after a colonoscopy is mild and resolves on its own.
A: After a colonoscopy, some patients may notice a small amount of blood in their stool or when wiping. This is usually considered normal, especially immediately following a biopsy or polyp removal. However, if bleeding persists, becomes significantly heavier, or is accompanied by other symptoms, it is important to consult your gastroenterologist.
A: You should seek medical attention if you experience heavy rectal bleeding (more than a few tablespoons), blood clots, severe abdominal pain, fever, or persistent dizziness or weakness. These symptoms may indicate complications that require immediate evaluation by a healthcare professional.
A: Any bleeding after a colonoscopy should typically resolve within a few hours to a few days. If bleeding lasts longer than this or increases in severity, you must contact your gastroenterologist for further assessment.
A: To minimize the risk of bleeding, it is crucial to follow your doctor’s pre- and post-procedure instructions. This may include dietary restrictions leading up to the procedure, hydration, and avoiding certain medications that may increase bleeding risk, such as blood thinners. Discuss any concerns and your medication list with your gastroenterologist before your colonoscopy.
—————————————————————————————————————
Karim Shakoor, M.D. is a board-certified gastroenterologist and founder of Colon & Digestive Health Specialists, LLC. He completed his residency and fellowship at Cook County Hospital, which is known for having one of the most extensive programs in the country. Karim Shakoor, M.D. is dedicated to providing his patients with the highest level of care to improve their quality of life. He specializes in the treatment of digestive disorders, including abdominal pain, colon cancer, constipation, diarrhea, diverticulitis, gas, gastrointestinal bleeding, heartburn, irritable bowel syndrome, peptic ulcers, swallowing difficulty, and ulcerative colitis.
Schedule an appointment | Google Maps | Services| About Us
© 2024 All Rights reserved © 2024 by Colon & Digestive Health Specialists