Diverticulosis and diverticulitis are two of the most frequently misinterpreted conditions in the complex terminology surrounding digestive health issues. Despite their close relationship, these conditions have different traits, symptoms, and approaches to treatment. Everything you need to know about diverticulosis vs. diverticulitis will be covered in this guide, including causes, symptoms, treatment, complications, and prevention.
What Is the Difference Between Diverticulosis and Diverticulitis?
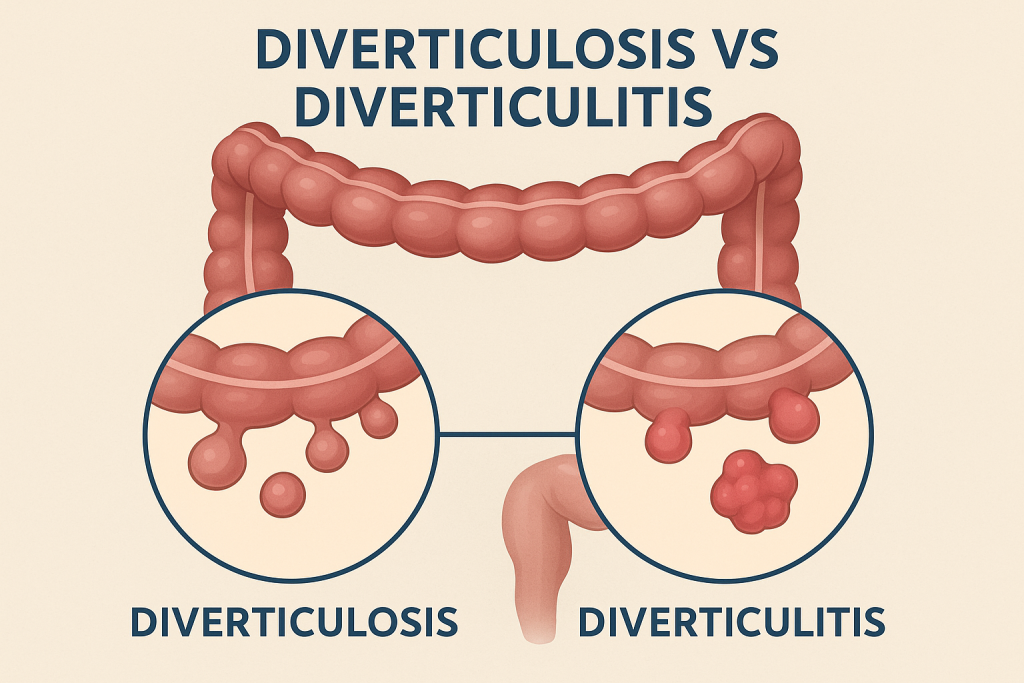
It is helpful to start with the colon (large intestine) in order to comprehend the distinction between diverticulosis and diverticulitis. Small pouches may occasionally form along the colon’s walls as a result of pressure. We refer to these as diverticula.
- Diverticulosis is the presence of these small pouches (diverticula) in the colon.
- Diverticulitis occurs when these pouches become inflamed or infected.
Diverticulosis is frequently found during routine colonoscopies and is typically asymptomatic. Diverticulitis, on the other hand, is a painful and potentially dangerous condition that arises when a diverticulum becomes inflamed or ruptures.
Diverticulosis and Diverticulitis Symptoms
Symptoms of Diverticulosis
The majority of diverticulosis patients show no symptoms at all. However, in certain situations, minor symptoms could include:
- bloating
- mild discomfort in the abdomen
- Modifications to bowel habits (diarrhea or constipation)
Due to their lack of specificity, these symptoms are frequently confused with those of other digestive disorders like IBS.
Symptoms of Diverticulitis
When diverticula become inflamed or infected, symptoms can become much more severe and may include:
- Persistent abdominal pain (usually on the lower left side)
- Fever and chills
- Nausea or vomiting
- Constipation or, less commonly, diarrhea
- Bloating and tenderness
- Loss of appetite
In some cases, the symptoms can be sudden and intense, requiring immediate medical attention.
What Causes Diverticulosis and Diverticulitis?
Causes of Diverticulosis
Diverticulosis is frequently associated with:
- A diet low in fiber causes harder stools and higher colonic pressure.
- As people age, the risk rises after age 40.
- Absence of exercise
- Being overweight
- Genetic susceptibility
Diverticula are more likely to develop in Western nations, perhaps as a result of inadequately fiber-rich diets.
Causes of Diverticulitis
Diverticulitis develops when diverticula become blocked with stool or bacteria, causing inflammation or infection. Risk factors include:
- Smoking
- Obesity
- Sedentary lifestyle
- Use of NSAIDs (like ibuprofen)
- Chronic constipation
Diverticulitis Complications You Should Know
Although rest and medication can often be used to treat mild diverticulitis at home, improper treatment can lead to serious complications. These could consist of:
- Formation of Abscesses :The colon may develop pus-filled pockets that need to be drained or treated with antibiotics.
- Perforation: Peritonitis, a potentially fatal abdominal infection, can result from a hole in the intestinal wall.
- A fistula: The colon and other organs, like the bladder or uterus, may develop an aberrant connection.
- Obstruction of the Bowel: The colon may narrow due to inflammation or scar tissue, making it difficult for stool to pass through.
- Bleeding: Diverticula can occasionally bleed, which can result in anemia or rectal bleeding.
Diverticulitis Diagnosis and Treatment Options
Making a diagnosis
- A medical professional may suggest the following if diverticulitis is suspected:
- Physical examination (looking for soreness in the abdomen)
- Blood tests to check for infection symptoms
- CT scan to verify perforation, abscess, or inflammation
- Colonoscopy to evaluate the colon (usually performed after the inflammation subsides)
Treatment for Mild Diverticulitis
- Most uncomplicated cases can be treated at home with:
- Oral antibiotics
- A liquid or low-fiber diet to rest the colon
- Pain relievers (acetaminophen, avoiding NSAIDs)
Treatment for Severe Diverticulitis
Hospitalization might be necessary if symptoms worsen or complications arise. Among the possible treatments are:
- Intravenous antibiotics
- Management of fluids and electrolytes
- Emptying abscesses
- Surgery to treat complicated or recurring diverticulitis
Colon resection is a surgical procedure in which the damaged colon is removed and the healthy sections are reconnected.
Diverticulitis Outlook and Prevention
Outlook
The severity of diverticulitis affects the prognosis. With the right care, the majority of people recover completely from mild cases in a matter of days to weeks. About 20% of patients, however, might have recurrent episodes, and a tiny proportion might get complicated or chronic diverticulitis that needs surgery.
Prevention
The best strategy is to control risk factors in order to prevent diverticulitis:
Consume a Diet Rich in Fiber: Fiber lowers colon pressure and softens stools. Consume fruits, vegetables, whole grains, and legumes on a daily basis.
Drink plenty of water: Fiber passes through the colon more easily when you drink enough water.
Engage in Regular Exercise: Exercise lowers inflammation and enhances bowel function.
Steer clear of NSAIDs and smoking: Both may raise the chance of complications or inflammation.
Keep Your Weight in Check: Diverticulitis risk has been associated with obesity.
Probiotics and Gut Health: Although further research is required, new findings indicate that preserving a balanced gut microbiome may help prevent diverticulitis.
Conclusion:
The Role of Colon & Digestive Health Specialists in Managing Diverticulosis and Diverticulitis
At Colon & Digestive Health Specialists , we are dedicated to delivering expert care for the prevention, diagnosis, and treatment of diverticulosis and diverticulitis. Our skilled gastroenterology team uses advanced diagnostic tools and personalized treatment plans to help patients achieve the best possible outcomes.
Whether you are managing diverticulosis or recovering from an episode of diverticulitis, early evaluation and proactive care are key to preventing complications. Take control of your digestive health today—schedule a consultation and let our specialists guide you toward a healthier, more comfortable future.
Dr. Karim Shakoor, M.D. is a board-certified gastroenterologist and founder of Colon & Digestive Health Specialists, LLC. He completed his residency and fellowship at Cook County Hospital, which is known for having one of the most extensive programs in the country. Karim Shakoor, M.D. is dedicated to providing his patients with the highest level of care to improve their quality of life. He specializes in the treatment of digestive disorders, including abdominal pain, colon cancer, constipation, diarrhea, diverticulitis, gas, gastrointestinal bleeding, heartburn, irritable bowel syndrome, peptic ulcers, swallowing difficulty, and ulcerative colitis.
